CLIENT Case study
Finding The Flow
How Davis Medical Center Makes Better Connections With Patients Thanks To Its New Patient Access Center And Registration Process
reduction in prescription refill time
reduction in insurance denials
Key Results:
- The rate of patients calling and speaking to a clinic staff member increased from 63% to 95%
- Insurance denials due to registration and coding errors dropped by 30%
- Prescription refill time fell from 1 week to 2 days
- Patient satisfaction and staff morale are increasing
- Capacity to see more patients daily has increased
- Learnings from the Patient Flow Initiative are being used to inform the $2.5 million Emergency Department re-design
The Problem:
“The lack of systematic processes led to problems in staff and patient satisfaction, billing, workflow and finances.”
Elizabeth Teets, Process Excellence Lead, Davis Medical Center
Tucked in the mountains of Elkins, West Virginia, the 90-bed Davis Medical Center (DMC) was facing some serious uphill battles in outpatient registration.
Clinic staff spent so much time doing non-patient-facing work, they didn’t have the capacity to deeply focus on all of their patients. Patient phone calls went unanswered and messages unreturned, causing patients to look elsewhere for help. Nurses were frustrated, having to take time away from patients to answer calls, and orders moved slowly through a cumbersome paper trail. The central scheduling process was inconsistent. Registration forms were different in each outpatient clinic, leading to errors, missing information, denied insurance claims, unnecessary follow-up with patients to correct errors, and lost revenue.
On top of that, orders in Electronic Medical Records (EMR) were still being hard-copied, faxed and filed, wasting valuable time and resources. And although a patient portal called Access My Chart existed, few patients or staff were using it, adding to the communication logjam.
Not surprisingly, staff morale was low and so was patient confidence.
The leadership:
“The approach we are using, with the facilitation of Value Capture, is completely different than programs used here in the past. I have seen this type of process change work, and fully expect the same results here at Davis."
-Vance Jackson, CEO, Davis Health System
Fresh thinking came with the arrival of new CEO Vance Jackson. Jackson had experienced the positive outcomes of Lean methods in a previous position. Although some of the Davis staff was skeptical because past change efforts had failed to stick, the new CEO was convinced that Davis Medical Center could change dramatically, in a way that would positively impact patients and staff for years to come.
Jackson created the Patient Flow Initiative to focus on registration and workflow in three outpatient clinics: Outpatient Services, Pediatrics, and Family Practice and Women’s Health. He chose a dedicated Improvement Team of eight staff members (six of whom worked on the Initiative full time, and two who worked on the Initiative part time) to lead the charge. He also tapped Value Capture to guide them through the planning and implementation of the Initiative.
The goal of the Initiative was to focus on patient access to outpatient and physician services from the point of need, to registration, until entry into the service area. In other words, the Improvement Team would work with Value Capture to make it easy for patients to connect with the clinics, and would make patient visits more efficient and meaningful.
The discoveries:
In just one month, 37% of patient calls made to the Family Practice went unanswered and without a message being left, 73% of messages left by patients could have been resolved using the patient portal, 276 insurance claims were denied, and more than $320,000 in insurance claims were denied.
Using Value Capture’s guidance and framework, the Improvement Team performed Operator Analysis in two patient access areas. By videoing people doing their jobs, measuring the time it took to perform tasks, counting the times paper was touched and moved, measuring patient wait times, and more, they carefully studied each process step by step. They collected and analyzed data on phone calls, Access My Chart usage, patient complaints, and processes like scheduling, registering, referrals, test authorizations, medication renewals, order management and more.
What they learned was eye-opening.
There were inconsistent protocols for registration, which led to costly mistakes in coding, as well as insurance denials and lost revenue. Different doctors had their own scheduling preferences, which led to confusion, re-scheduling, double-bookings, and scheduling invalid procedures. And because there weren’t employees focused solely on non-patient-facing work, patients both at the clinics and on the phone weren’t getting the information they needed.
The solution:
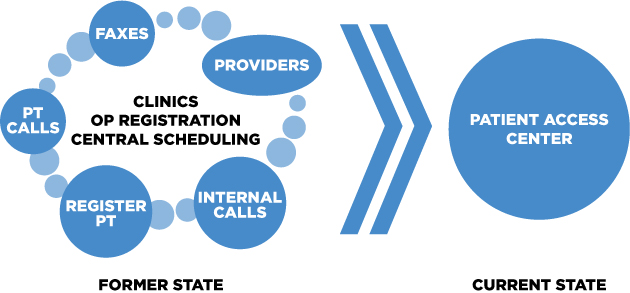
Create the Patient Access Center to segregate non-patient-facing work, establish consistent registration protocols, create a unified scheduling system, and help patients utilize Access My Chart.
Now that the team understood what was really happening in their clinics, they were in the right position to create an effective approach.
With Value Capture’s coaching, the Improvement Team devised a transformative solution. They created the Patient Access Center (PAC), a behind-the-scenes communication hub comprised of 50 staff members combined from the various areas related to patient access, dedicated to helping patients over the phone.
Displaying confidence in and commitment to his team, Jackson offered an unused area for the new PAC. He made sure the team was highly engaged in designing and furnishing the space. New hires, new protocols and staff training were put in place.
Throughout this process, Jackson and other DMC leaders met with the Improvement Team, at least once daily, to provide the help the team needed to keep moving forward.
The team designated three levels of staff within the PAC: Telephone Representatives, Patient Access & Scheduling Specialists, and Clinicians. The Telephone Representatives are welcoming voices who put patients in touch with the right PAC resources. They also take messages within EMR, tasking them to the appropriate PAC resource for a timely response. Patient Access & Scheduling Specialists handle scheduling and registration using newly standardized systems. And Clinicians are nurses who are dedicated to helping patients with questions, test results and prescription renewals over the phone.
Segregating these non-patient-facing responsibilities allowed the patient-facing staff in the clinics to focus wholly on patients coming into the clinics for appointments. This made it much easier for patients to see their providers, and get tests and lab work done more efficiently. Newly standardized registration protocols nearly eliminated coding errors, cutting rework and insurance denials significantly.
Using more out-of-the-box thinking, the team devised incentives for the PAC staff to cross-train. The more skills staff members acquire, the more promotions and salary increases they enjoy. This enables more flexible scheduling of Patient Access and Scheduling personnel throughout Physician Practices, Outpatient Registration, and the PAC itself. It allows for the ability to have team members step in where needed, and also energizes staff and raises morale.
In addition, orders are no longer hard-copied and moved physically, but electronically processed in EMR, reducing wasted paper and time. And with the help of the Davis Marketing Team, the Improvement Team is promoting greater patient use of Access My Chart, ensuring better communication as well as faster scheduling and prescription refills.
“By separating non-patient-facing activities from check-in, we can move the work to people who have the resources and time to handle them properly.”
David Tener, Value Capture
The results:
“A small team of employees with knowledge of the many areas that contribute to patient access has created a solution to eliminate many of the causes of patient dissatisfaction.”
Vance Jackson
In just 18 weeks, the DMC Improvement Team, along with Value Capture advisors, identified and analyzed problems in patient access areas, and created and implemented solutions that are already providing terrific results:
- Unanswered phone calls dropped from 37% to 5%
- Denied insurance claims dropped 30%
- Use of Access My Chart for messaging jumped an average of 72%
- Prescription refills handled in 2 days versus 1 week
- Telephone messages are returned in an average of 12 minutes and 30 seconds, versus 2 days
- Physicians, nurses and other providers have welcomed the improvements, and are able to spend more quality time with patients
- Capacity has grown, with Physician Practices now able to see more than 300 patients a day
What’s more, DMC is receiving fewer patient complaints. Questions are answered in real-time. Patients are adopting the portal at a faster rate. Morale has improved. And the workload has leveled.
“Our employees are also our patients so there is a great opportunity for real time feedback. People are stopping me in the hall and saying, ‘I called the PAC and got right through. I had an appointment in just a few minutes!’”
Elizabeth Teets
Team members report that acceptance of the change is rising dramatically. In fact, nurses have embraced the opportunity to work in the PAC. And PAC staff is voluntarily coming in on Saturdays for training to improve their skill sets. In addition, new employees are able to be trained much more easily and consistently than before. Each addition to the team helps to perpetuate the new culture.
Other departments throughout the hospital have also jumped in to help with the initiative, from Support Services and Information Technology to Human Resources and Marketing.
Davis Medical Center now has numerous advocates across clinical and administrative departments to help spread the value and practical applications of Lean process across other areas of the hospital, as members of the Improvement Team have learned to be Lean improvement coaches, with the help of Value Capture.
“There’s been a change in our culture, and we have a better organization because of it.“
Elizabeth Teets
Continuous improvement:
“When we start tearing down walls and examining connections between hospital areas and functions, things really start to fall into place. People begin to understand where they fit in the whole value stream continuum and they see opportunities to help each other meet the patient’s need and make their own work life more fulfilling and less stress-filled.”
David Tener
The positive impact did not stop at the end of the project. Since the Patient Access Initiative, Physician Practices has added four additional providers and are seeing over 300 patients a day on a regular basis. This capacity increase would have been unthinkable before the project.
Emergency Department and Inpatient follow-up appointment slots, as well as same-day acute visits, have been standardized across all providers. This added availability gives established patients much greater access to primary care when they need it most and has eliminated the need for a separate transitional care department.
Ancillary departments, such as outpatient lab, have seen the benefits of partnering with the new system and are piloting taking over responsibility for entering their own orders. This change has resulted in getting patients through the registration process even faster by eliminating rework, which was a major time and quality constraint before.
Next steps:
“This is the first of many areas of Davis Health System that will be looked at with a critical eye. Employees need to be invested in continuous process improvement and the lasting effect it has on maintaining healthcare in our community.”
Vance Jackson
Jackson is now turning his attention to a $2.5 million re-design of the Emergency Department, building on and applying the lessons learned during the Patient Flow Initiative. Although the E.D. project is in the preliminary blueprint phase, Jackson is already using process improvement methods to inform construction.
Jackson is not only interested in changing the brick-and-mortar, he’s also interested in making the emergency room experience better for the people served by Davis Medical Center.
Vance Jackson, the other Davis leaders, the Improvement Team, and everyone at DMC are committed to quality, patient-friendly healthcare, and they are using Lean principles to help deliver.
Podcast with Vance Jackson
Vance Jackson talks about the benefits he and his fellow leaders enjoy when they go to nursing units, the E.D., and other areas where patient care is delivered, where they silently observe the work that is done. Hear Mr. Jackson talk about many other learnings in building and deploying the Davis Way, the way he now thinks about safety (for patients and staff), and the focus Davis Health System will take in its improvement journey, in this podcast with Mark Graban.
Ready to start a conversation with Value Capture?
We'd love to talk with you about the challenges you're facing.