Value Capture Opportunity: Testing the VC System in a Service Line
OPPORTUNITY: TESTING THE VALUE CAPTURE SYSTEM IN A SERVICE LINE
Test the Value Capture system by redesigning any service line.
Summary
- Key service lines often contain unnecessary complexity which leads to a less than perfect patient experience and excess costs that can be reduced by 30-50%. A hospital-based Cardiac Cath Lab provides an excellent example.
- Utilizing the Value Capture System to redesign how your Cath Lab or any other key service line operates can create the foundation for your future business case by teaching your hospital how to achieve maximum quality, minimum waste, and minimum lead-time in any process.
- Value Capture has an extensive track record helping health systems redesign elements of their care delivery pathways to achieve this business case.
For leaders seeking to transform their hospitals
Determining the right transformation strategy is one of the most important decisions any CEO makes. Value Capture understands this. Although we believe that organizational transformation cannot take place through a series of projects, we do believe that starting with a manageable slice of the organization is a potential starting point in determining which path to choose to capture all of the value in your organization. Value Capture has partnered with hospitals to do groundbreaking work to eliminate infections, build safety and efficiency into medication delivery and other inpatient work that has shown that highly safe and reliable processes operate at lowest cost. The shift in care to the outpatient arena and the degree to which hospitals depend on the success of these services for their overall wellbeing makes the ambulatory care setting and similar service lines excellent opportunities to demonstrate what is achievable. We are confident that by allowing us to work directly with you (the CEO) and your team, you will see the power of the Value Capture System to transform any service line and its potential to do so across the entire organization.
What makes our approach different?
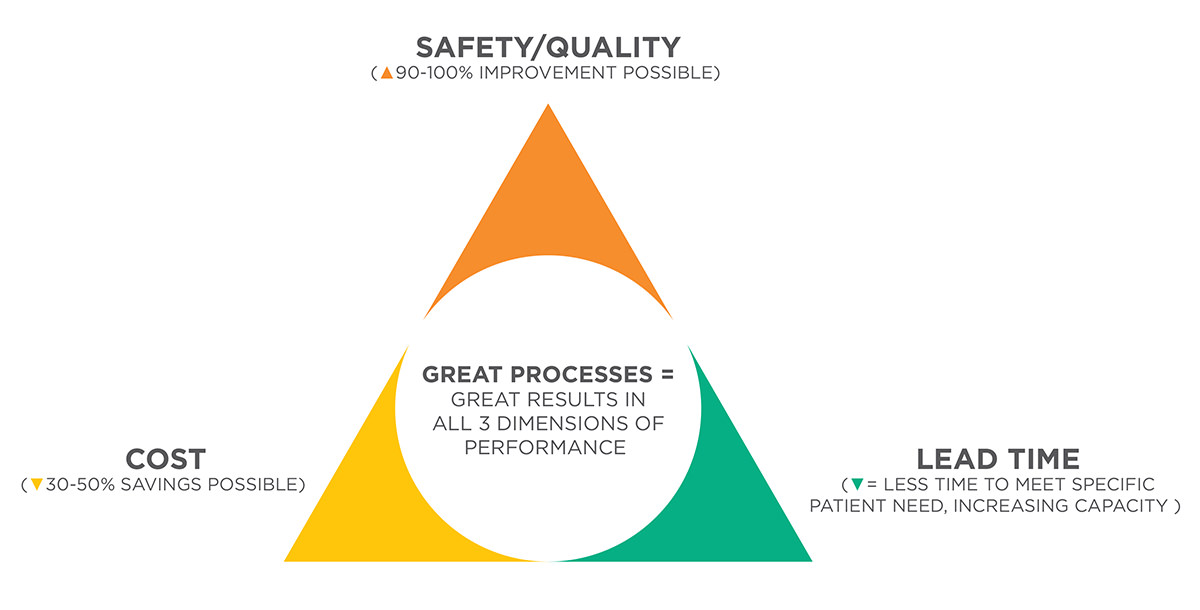
Rather than specializing in one inpatient or outpatient service line, we specialize in deeply understanding process design as it applies to any service. We will work with you and your staff to characterize and seize the opportunity in any service area that is core to your business case, and learn to do it for all others. Possible targets include, but are not limited to, Cath Lab, Oncology Services, Wound Clinic, Pain Clinics, Medication Delivery Systems, and many others. Based on our track record we are certain that we can show you improvement in three performance dimensions that are typically thought to require trade-offs: cost, safety/quality and lead time.
Business Case Example:
The Cardiac Catheterization Lab
Quality Opportunity:
Traditional measures for quality in the cath arena exist, including mortality rates, complication rates and “door to balloon” times. However, a huge untapped benefit lies in addressing quality/safety issues that are built into the system and currently seem unavoidable. Examples include delays in care due to the unavailability of previous results, last-minute revelations about clinical circumstances (relevant prior surgeries or diagnoses), or not having the exact supply that is needed at the time it is needed. The time spent working around these problems is time taken away from direct patient care and stresses the process. All of these seemingly “small” problems can be eliminated, creating a safer patient experience and substantially increasing throughput in the lab. Additionally, the impact of delays on patients and families adds undue stress at an already difficult and often scary time. Patient satisfaction falls despite the service recovery efforts of conscientious staff.
Cost Opportunity:
Based on past clients and current Medicare statistics the average cost for an average outpatient cath procedure is $1,150 and Medicare reimbursement for 2009 is $2,600, providing an attractive margin. Inpatient reimbursement is more difficult to calculate, but for the purposes of this example we are focusing on percutaneous procedures encompassed in DRGs 248-251 which pay $12,578 on average depending on complications and comorbidities. Given most hospitals are price takers, a decrease in cost is the only way of increasing per case margin. We can help you decrease non-personnel costs by 30% in this or any pathway.
Cath labs typically have 300-350 specific supplies on hand. Certain supplies such as drug eluting stents are very expensive. There is a hidden opportunity to increase cash on hand by gaining an understanding of the true demand for these materials and matching the inventory accordingly. Inventory cost can get hidden in certain financial ratios which rely on “costs of goods sold” or other accounting based ratios which consider inventory an asset. In Taiichi Ohno’s book, The Toyota Production System, Beyond Large Scale Production, Ohno scoffs at the fact that accounting standards count inventory as an asset and employees as liabilities. If you do not purchase what you do not need there is more cash available. This increase in “days cash on hand” can be used to pay off expensive debt or saved to improve bond ratings. Whatever path you choose there is a business benefit to create systems that reduce inventory and avoid spending for products that are not immediately needed by a patient.
Another major financial concern that hospitals are facing is the CMS expansion of RAC audits. The Cardiovascular Service line is one of the areas that can be most prone to penalties. Many of the audits are a result of medical necessity denials. Ensuring the information is correct and available is often thought of as its own process instead of a component of the pathway. As Value Capture helps you to draw out the current condition in its entirety, all aspects of the pathway are considered (including the steps that relate to the revenue cycle) and can be improved.
Lead Time Opportunity:
By decreasing lead time – the amount of time from when a need is identified to when that need is met – patient throughput increases. Based on the current average outpatient margin of $1,450, if a facility is able to add just one more procedure per day this would translate into an additional $377,000 in profit for the hospital per year independent of any cost reduction opportunities. Both pre-specified and unplanned inpatients have a direct impact on the lead time for the entire Cath Lab. For example, if an inpatient who could otherwise be cared for on the inpatient unit is in recovery waiting for a bed, a bottleneck can occur, especially impacting a lab that uses the same bays for prep and recovery. Using techniques to smooth out the peaks and valleys in patient demand will increase the Lab’s capacity, capturing an opportunity cost on the missed cases.
What would this process produce?
- Exact quantification of patient need the core process or service line must deliver against
- Measures of the system’s ability to meet those needs as measured in current quality, safety, cost and lead-time information
- Measures of the spread between resources actually consumed by patients and resources purchased by the institution (a prime source of hard-dollar savings and clues about how the processes can be better linked to actual patient need)
- Assessment of variability within specific work processes and their impact on quality/safety, cost and lead-time
- Assessments of the overall complexity of the service and opportunities to simplify the design and to deliver additional goods and services over the same process “pathway”
- Assessments of the current ability of the people doing the work in the service or process to effectively solve problems in order to keep the process stable, producing highest quality results at the lowest possible cost
- Assessment of how level the work flow is, with correlating impacts of surges in demand on lead time, quality and cost
- Assessment of the degree of lead-time currently built into the system and its impact on resource waste and ability to meet patient need
- Assessment of batch sizes currently employed in the services and corresponding impacts on efficiency and ability to meet patient need
- Facilitated redesign sessions with the people that do the work and the people with operational authority over the work, addressing all elements of the above assessments
- Updated measurements (will require ongoing work by hospital)
Proposed Timeline
The process of analyzing and supporting changes to capture the opportunity will take 3-4 months to complete. The proposed timeline will vary based upon individual circumstances but tend to follow the following pattern:
- Pre-week- one on one meeting with CEO
- Week 1-Initial meeting describing the characterization; must include Chairs, appropriate managers, CFO and other relevant parties
- Week 2- Introductory planning session to develop an A-3 (The A-3 is a planning methodology that Toyota developed which utilizes the scientific method.)
- Week 3-6
- Observation (teaching a select group of people that do the work)
- Collect Financial, Volume and Case Mix data
- Develop a current condition with problem list and opportunity analysis
- Week 7-8 – Complete Target Condition/begin redesign
- Week 9-15 TBD based on problems/opportunities identified
- Week 16 - Wrap up meeting (pending scope could be as early as week 12)
The skill set developed through this type of encounter applies to the improvement of any other pathway.