FEATURED Case study
Improving Patient Experience through a New Primary-Care Process at Sutter Health
reduction, check in to rooming
length of stay reduction
of breaks taken (up from 6%)
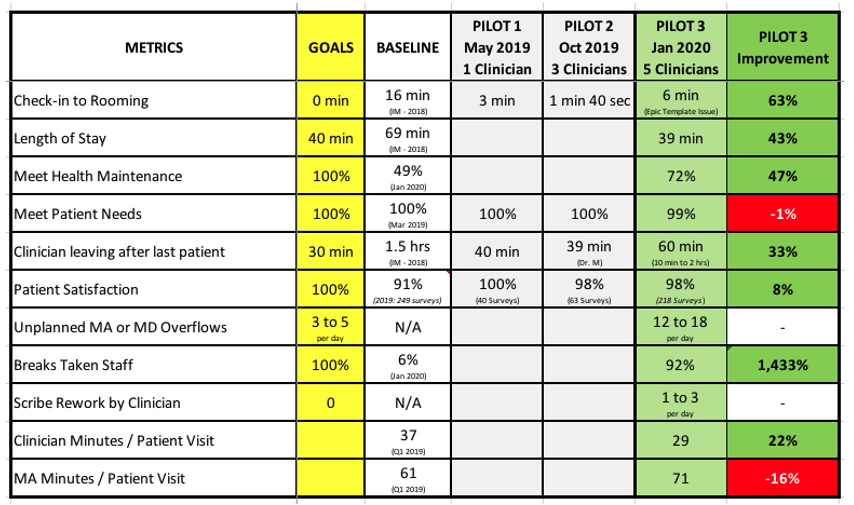
Key Results:
- 63% reduction check in to rooming
- 43% LOS reduction
- 47% increase in Meet Health Maintenance
- 33% reduction in time from last patient gone to providers going home
- 8% increase in patient satisfaction
- Breaks taken increased from 6% to 92%
“Our traditional practice model in primary care was antiquated. It was not efficient, we knew we could provide better quality and safety of care to our patients, and it was distressing to the clinicians and staff…. We knew we had to change.”
Dr. Mike Conroy, Chief Medical Officer, Sutter Medical Group (part of the Sutter Health network)
“Conditions were leading to increased burnout and clinician, patient, and staff dissatisfaction. [We] recognized that we’re getting to a boiling point, and there’s a sense of urgency that we need to address this.”
Dr. Ali Mokhlesi, physician in the Internal Medicine care center
Sutter Health has a long history providing award-winning healthcare services and striving for operational excellence. Its leaders, not content to rest on past achievements, set on a course to develop a new, improved practice design, specifically to address physician burn-out and turnover. The team had seen and was inspired by work being done at San Mateo Medical Center with the assistance of Value Capture. Understanding the achievements of San Mateo Medical Center led to Sutter seeking Value Capture’s help.
Sutter leaders (including entity executives) began work with Value Capture in a facilitated self-assessment. Through this experience, these leaders observed and more fully understood the current condition. While ongoing efforts had created improvements, some key components were lacking: leaders talked daily about problems, but tiered communications were missing due to gaps in the alignment of the work system, improvement system, and management system. The assessment also reinforced the idea that practice design developed only through the lens of physician satisfaction could lead to unintended consequences (such as negative effect on patients and employees in an attempt to speed the finish of work) and highlighted the need to bring in more patient and staff perspectives.
Thus the focus of the work expanded from the physician experience to a broader primary-care transformation. The changes sought would:
- Put the voice of the customer center stage in the care sites;
- Design improvements to patient flow that would enhance both the patient and physician experience; and,
- Develop systems and a culture for safety (physical, emotional, and professional) for learning, experimentation, and continuous improvement.
Plan for Primary Care Improvement
Sutter Valley Medical Foundation’s Education Street center in Auburn, California, was selected by a value-stream mapping team to kick off pilot projects, starting with the Internal Medicine center.
Along with a leadership steering committee, the mapping team developed a vision for an ideal flow in primary care and established goals of perfection:
- Zero patient wait time
- 100% health maintenance items addressed
- 100% patient needs met
- Provider and staff leave office within 30 minutes of the day’s last patient
- 100% patient satisfaction
A design and implementation team for the pilots was formed, requesting a multidisciplinary group of volunteers: patient service representatives (PSRs), medical assistants (MAs), registered nurses (RNs), and clinicians. “We were pleasantly surprised at the positive reactions and energy we got from the different parts of the organization when we asked for volunteers,” says Dr. Conroy. “And, secondly, we did emphasize as much as we could that frontline employees — both physicians and staff — [were sought more so] than managerial positions to participate in these work groups.”
Focus on Safety
“What changed was the true emphasis on safety that was encouraged by Value Capture…. That emphasis aligned with something that hadn’t been on our radar necessarily, which was teaching real-time problem solving to align staff and clinicians as part of the support of the whole project … We decided to focus a fair amount of our early training time and targets around safety.”
Dr. Conroy
Worker safety is a critical component of Value Capture’s transformation strategy, a belief that dates to when the late Paul O’Neill, a Value Capture leader, was the CEO of Alcoa. “Engaging first on worker safety is preconditional to developing employees’ psychological safety and the leadership coaching capability that are so necessary to transform the work,” says Didier Rabino, Client Advisor. “Employees need to feel physically safe and that their personal safety is respected in order to engage, without limitation, in continuous improvement.”
The Sutter Safe Care safety program has been part of the organization’s daily engagement system, but the pilots took the concept further. “One of the focuses is addressing physical, emotional, and professional safety,” says Carrie Putnam, Senior Lean Consultant with Sutter Valley Medical Foundation. “That work was really focused on making it safe for people to speak up and having an environment when people speak up it’s actually celebrated, encouraged, and recognized.”
Jennifer Ashley, Site Supervisor in Auburn noted that with the safety focus, staff begin to see things differently and connect their observations to real-time problem-solving and rapid improvements.
And the “ah ha” moment for her was realizing that the same problem-solving process wasn’t just for safety problems but could be effective for any issue they encountered.
“Safety is the best place to start to engage every employee in improving the work,” says Rabino. “It helps to develop the idea of a theoretical limit of zero safety incidents for workers and patients, eyes to see issues, and emotional and professional safety to elevate all problems in full transparency in real time. Safety is also a lever to develop not only problem-solving capabilities, but also coaching skills.” As employees become emotionally and professionally safe to point out and solve safety problems — without fearing a negative response — it leads to ingrained behaviors and the confidence to apply those behaviors to non-safety issues.
Understanding the Current State; Imagining an Ideal State
The cross-functional pilot team gathered information of the current state of primary care, Among other things, the pilot team learned that patients disliked waiting for their visit to start, for paperwork and prescriptions. Dr. Mokhlesi noted, “Many of us in the world of medicine, because of our own pressures and all the work we’ve got to do, we have even convinced ourselves that this is the nature of the beast. If you want to come see a doctor, you’ve got to know you’ve got to wait.”
In May 2019, during the first pilot, the team was challenged to envision an ideal future state with the theoretical limit (perfection) in mind. Value Capture asked the team to design or redesign processes to get as close as possible to the ideal state. Nine areas of improvement work were identified that would need to be solved before the ideal-state pilot could be brought to scale. The pilot team and local groups within the team determined how to address the nine improvement areas: use either real-time problem solving (RTPS) and experimentation or rapid improvement events (RIE).
The team’s desire and effort to get as close to the ideal state as possible, coupled with their clear-eyed current state understanding, safety focus and new problem-solving skills, enabled them to establish an ideal-state pilot that integrated work, improvement, and management redesign. Those collective elements produced many outstanding design outcomes:
- Takt time: This one-piece flow concept is common in manufacturing, where it refers to the pace of customer demand, but rare in healthcare, especially primary care. Patient visits were scheduled to begin at 7-minute intervals for the third pilot.
- Agenda setting: Standardized practices for MAs were designed to make the most effective use of patient visit time. As part of this, the most pressing issues or patient concerns would be addressed as early in the visit as possible so that subsequent patients would not be delayed because important questions arose when the patient visit should have been ending.
- Medical-assistant scribing: To further patient-centric services, MAs became scribes for the doctors. This enabled the doctor to focus on the patient, delegating computer work to the MA/scribe.
- Pull system: In order to ensure uninterrupted care of the patient during their entire visit, the role of an “MA/float” was defined. When something was needed in the room during the patient visit (e.g., a flu shot, materials, supplies, equipment), the MA/scribe contacted the MA/float using an electronic device and it was brought into the room by the MA/float.
- Synchronization of people flow: At a given scheduled time, a doorbell rang (a digital clock indicating minutes and seconds was placed above the doorbell to avoid variations) and the PSR pulled a patient into the visit and initiated the one-patient-flow process. To avoid patient wait-time in the exam room, the end of the MA/scribe rooming process was synchronized with the beginning of the doctor’s work. Once the MA completed taking a blood pressure, the MA sent a “two-minute warning” signal to the doctor. This gave the doctor two minutes to review the patient chart, including notes just taken by the MA/scribe, and enter the room just in time to continue with the next steps of the patient visit.
- Use of overflow: If a patient visit required an unexpected doctor consultation, an MA/overflow was signaled to start the rooming process with the next patient. In this way, full attention could be provided to each patient while maintaining the flow at takt time.
Systems for Operational Excellence
As changes were made to processes during the pilots, there was an underlying emphasis on alignment of three systems that guide continuous improvement. Each of the three systems is a collection of elements organized for a common purpose:
- The work system identifies how work is to be performed in order to add value to the customer; elements include the pathway of product/service delivery, process standard work, visual management, and material replenishment signals.
- The improvement system helps to identify and solve problems and make improvements to how work is performed; elements include problem identification, RTPS, help chain, and management of key performance indicators (KPIs).
- The management system supports employees doing and improving the work. It keeps those within the organization focused on and improving toward organizational goals; elements include alignment to True North, development of new KPIs, enabling problem solvers, standard work confirmation, leader standard work, and cross-training.
“The work system, improvement system, and the management system have to be aligned for this to work. I can’t stress how much that has to happen.” Changes to the management system to help during the pilots were “huge” and aligned individuals’ beliefs with process requirements and gave support to the people doing the work. “That is what our job is. They do the work, they know the best play, they’ve done it before. Listen to them and help develop them to be problem solvers.”
Jennifer Ashley
Possibly the Greatest Challenge is Change Itself
The work of the pilot team also identified many challenges that are common to healthcare transformation and that the Sutter Health care sites will likely encounter when the practice design is more broadly implemented.
“I think we’ve seen what is common in projects like this: change management, when it involves human behaviors, is particularly difficult,” says Dr. Conroy. “It’s true that almost no matter how many times and how many different ways you communicate the benefits of a change, the collaborative nature of the workflow and decisions, and the involvement of frontline staff, people respond to change in different ways… You just have to be diligent about your communications and understand how difficult and challenging it is.”
“Trying to get people to come to the same page is something we’re still struggling with,” adds Dr. Mokhlesi. He references a phrase used by Value Capture’s Rabino as to why consensus-defined standards are necessary, albeit difficult: “There can’t be two best ways… We hear a lot from our team members that ‘the way I do it is the best way.’ How could that be possible, that two totally different ways of doing things can both be best ways?”
Pilot Outcomes
At the completion of the third pilot, which involved five clinicians, the patient takt time had been reduced to 7 minutes — i.e., every 7 minutes a PSR brought a patient into the process. Lowering takt time reveals the efficiency of patient visits. It also enabled the care center to meet a customer demand of 72 patients in a work day, while still leaving one hour at the end of the day for a pilot debrief.
As important, the goals for the practice design had been improved significantly. For example, the patient length of stay had been reduced from 69 minutes (much of it is non-value-added) to 39 minutes (see Pilot Goals on the next page). Patients get 30 minutes of their life back while getting better value and a better experience.
“There’s no patient wait times, and that’s great,” says Ashley. “I think patient care is definitely high [and we’re improving] health maintenance. The quality is just so much richer — it’s just built all in there.” She adds that having MA/scribes has been a value to the clinicians and pleased patients, who appreciated that their doctor wasn’t distracted by computer work throughout their exam.
In addition to tangible improvements to metrics, favorable cultural results were achieved in the pilots: Staff were spending more time focused on patients and planning for the medical needs of patients — and not distracted by non-value-added activities. Clinicians were more likely to close charts on time and leave the center at a more acceptable hour. Staff came to believe they could experiment in the pursuit of perfection, seeing and solving issues they previously had not noticed. Pilot team members will forever see things differently, says Rabino. “Once you learn how to see, solve, and share problems, you’re hooked. You’re going to be problem-solving all the time. You never undo this learning.”
The team’s ability to experiment and develop changes that benefit the organization is unlikely to stop. “The team has much more confidence that they can actually design and put change into place,” says Dr. Conroy. “One of the fears the team had was that they would come up with great ideas that would be squashed by leadership or told it was impossible for one reason or another. I think they are surprised and delighted by finding that is not the case. There is sort of an esprit de corps, a morale that’s different among the team members involved.”
[This case study is excerpted from our white paper discussing this work. To learn more about Sutter Health’s primary care redesign, please click here to download the white paper.]
Ready to start a conversation with Value Capture?
We'd love to talk with you about the challenges you're facing.