Does the idea of perfect care, zero harm, or 100% compliance give you pause or make you nervous?
If so, you are not alone. It is tempting to follow the pack, conforming to the idea that we have to set goals that are conservative and "realistic" to ensure the metrics are attainable for this year’s incentives or that we do not "discourage" our teams. If we are serious about transformational improvement, then we need to push the boundaries of what we believe is possible. Rather than setting limits based on the benchmark or the national average for our improvement goals, we should aim for the stars, and then provide the leadership support toward making that happen. This approach challenges our teams to think about what is possible and opens the door to experimentation and innovation.
In this blog, we’ll conclude the series on patient flow improvement by discussing the importance of leveraging theoretical limit thinking and continuously experimenting towards ideal.
Pitfall: Thinking there must be tradeoffs: staff and physician workflow and satisfaction vs. patient experience vs. cost/reimbursement vs. quality/readmissions
Healthcare organizations often face difficulties with patient throughput improvement efforts because of perceived tradeoffs. For example, successfully decreasing length of stay could also result in increased 7-day or 30-day readmission rates and reduced insurance reimbursement. Likewise, staff and physicians may feel stressed from trying to get patients discharged by noon, while the patients may feel rushed out of the hospital. It can seem that improving patient flow is a two steps forward, one step back proposition.
In addition, healthcare organizations will often use external benchmarks to inform goal setting: “top decile performance is this level, so let’s set our target there.” Understanding where your organization is performing relative to other similar organizations can be beneficial when used appropriately, such as gaining context to better understand your current condition. However, it becomes problematic when people use benchmarks to justify maintaining performance, stifling improvement: “We’re 98th percentile, it’ll be nearly impossible to be any better!” But who wants to be cream of the crap? More importantly, what level of performance do your patients deserve? Imagine that this data represents surgical site infection rates or the rate of misread lung cancer CTs. Translate that data to the actual number of patients affected...and then decide who wants to be the one with a surgical infection that requires a secondary surgery or misdiagnosed lung cancer that progresses to Stage 4 without being treated.
Do this instead:
Strive to set goals based on the theoretical limit, pushing beyond benchmarks.
Aim to eliminate avoidable admissions.
Habitually excellent organizations benchmark against themselves and continuously seek perfection, striving to get closer and closer to the theoretical limit of performance, such as zero harm for patients and staff, 100% patient satisfaction, 100% employee retention, zero wait or waste, etc. The benefit of this approach is that it unlocks innovative thinking by creating the necessary tension to truly improve processes and remove waste, rather than simply working harder to try to meet goals—it aligns everyone in an aspirational way. In the context of patient flow, you might apply theoretical limit thinking in different ways, such as seeking to eliminate avoidable admissions or progressing care at the rate of patient healing.
Avoidable Admissions
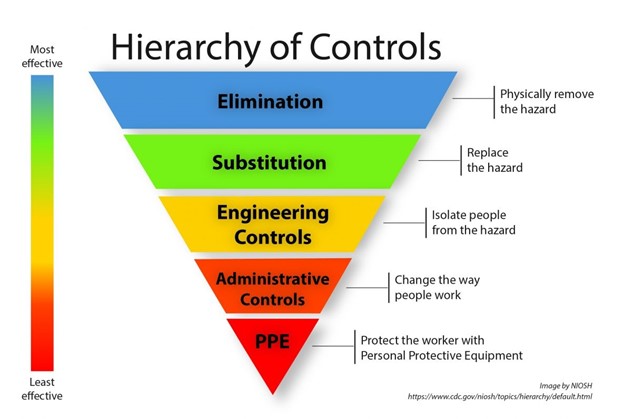
In the Hierarchy of Controls, elimination is the most effective level of protection from hazards. Applying this thinking to patient throughput: What if the patient never needed to be admitted to the hospital in the first place?
Your hospital likely has some level of avoidable admissions. Seeking to eliminate such admissions can have multiple benefits, from opening bed capacity in the hospital to decreasing costs for the patient and the health system. And you don’t have to worry about the balance between length of stay and readmissions if these patients don’t have to set foot in the hospital!
Further, unlike working on length of stay, aiming to eliminate avoidable admissions drives systemic improvement by involving all areas of the health system, not just hospital-based teams. What would have to be true to avoid having to admit these patients? Perhaps your organization finds opportunities to improve primary and urgent care access, strengthen transitions-of-care processes, or engage your home health team to deliver acute care in the home.
Pace of Patient Healing
What if admitted patients were able to go home as soon as they were healed? One organization with deep connections to Value Capture applied this theoretical limit thinking to its patient flow improvements, designing, piloting, and spreading a patient-centric collaborative care model. On the pilot units in this model, the patient’s RN became the proverbial quarterback of the care team, leading a care conference that always included the attending physician and the pharmacist, and often included specialists, physical therapy, and other ancillary care team members.
Once the care team agreed on the plan of care and the criteria for triggering the next plan (e.g., patient’s hemoglobin level reaches x grams per deciliter), the nursing team (primarily the LPN and aide, whenever possible) would execute the plan, with the RN monitoring the patient’s progress against the criteria and ensuring critical care tasks were completed on time and accurately. The collaborating team came together minimally every 24 hours but strove toward the theoretical limit—coming together at the pace at which the patient was healing, which could be 12 hours, 8 hours, or even earlier. In some cases, the team could proactively queue up the next plan of care, obviating the need for the care conference.
This approach was so successful that all medical units moved to the collaborative care model, and all newly hired nursing staff completed foundational training on a collaborative care unit prior to going to their home unit to complete their orientation.
(Note that a helpful measure here is relative length of stay [actual minus expected], where zero indicates that the patient stayed exactly as long as the geometric mean.)
Experiment towards ideal (safe, high-quality care that meets patients’ needs, without waste) to achieve no-tradeoffs improvement.
Regardless of which approach you take, it is critical that you apply scientific method, plan-do-check-act (PDCA) thinking to continuously improve the processes that impact patient flow and share learnings with other units or teams who can benefit from your improvement. Aiming for the ideal—physically and psychologically safe for all; defect free/right the first time; meeting each patient’s needs one-by-one, immediately, on demand; without waste—keeps everyone focused on delivering the most value for the patients while also making it easier for staff to do the work.
- What is the ideal (theoretical limit)?
- Where are we now?
- What is our next target condition, and by when?
- What obstacles are preventing us from getting there? Which one will we work on now?
Continuing to apply this thinking and running experiments to test countermeasures to the root causes of the obstacles drives progress towards no-tradeoffs, win-win-win improvement. The organization mentioned above experimented towards ideal with its collaborative care model to deliver outstanding results: the pilot unit achieving greater than a one day reduction in length of stay, no increase in readmissions, zero medication reconciliation errors, and increased staff retention.
We can improve patient flow, with no compromises, by approaching the work as a complete system. Challenging our teams to find innovative solutions that improve their worklife while still getting the results our patients deserve. Setting a goal at the theoretical limit does not require getting there in one step, it is a journey. Get inspired and commit to a journey centered around excellence rather than settling for just better than the competition.
Want to learn more about improving patient flow and the impacts it can have? Check out our webinar recording with Legacy Health leaders, "Strategies for Reducing Length of Stay in Hospital Settings." Also see our blog posts: "Unlocking Patient Flow: Empowering Frontline Caregivers for Sustainable Solutions"; "Navigating Patient Flow Challenges: A Lean Approach to Root-Cause Problem Solving"; and, "Optimizing Patient Flow: Avoiding Silos and Embracing Systemic Thinking in Healthcare."
This blog was a collaboration between Senior Advisors, Alison Hartman and Anthony Pepe.

Written by Value Capture, LLC
We are consultants who act as trusted advisors that guide health systems determined to produce perfect health with zero harm, wait, or waste — for patients, teams, and communities. We work with organizations by solving their biggest problem and doing it in a sustainable way, with “no tradeoffs” leading to exceptional change in organizations and the knowledge to continue to improve.

Submit a comment