Recently, Value Capture hosted "Applications of Lean Leadership Methods in Home-Based Care," our webinar with Duke HomeCare & Hospice (DHCH) leader, Cooper Linton.
In this outstanding webinar, Cooper shared the successes and challenges DHCH has faced as this Duke Health agency sought to improve a number of systems and processes as part of its commitment to zero harm for all.
This post provides just a few of the highlights from this discussion. Click the image below to get the recording, slides and more.
Respect is an Action and Vital Element of Zero Harm
As a “fundamental” element to begin its Lean journey, Cooper said, with "an intrinsic respect for our staff... that turns into an action of how we guard, use, protect a resource – the time of our staff and their expertise.
"We were also focused around ‘Commit to Zero...,’ the idea that no one should be hurt in the provision of care or in the receipt of care. We wanted to eliminate waste, error, rework, and that ties back to respect for time.”
Unpacking “Commit to Zero,” Cooper explained that, “We wanted to include harms to people’s loved ones. They’re caregivers in the home, the emotional state of those people, [and] obviously our staff, and then our business. And we began to look at risk differently, and look at, what does it mean to be focused on risk? We’re really going to focus, thinking about how do we address risks to keep them from ever becoming harms.”
Tiered Huddles: Timely Communication to Raise and Solve Problems and Support Staff
“The most tangible way [to roll out Lean principles] was to begin to put in a series of safety huddles, or what we call tiers.”
“Tier one is our frontline staff... And the idea was to prioritize the feedback of that staff, what they needed to do their work, to clearly identify safety issues. Right then, right now, there’s a sense of urgency in that and understanding of what they needed for the support of their work.”
"And the idea was to prioritize the feedback of that staff, what they needed to do their work, to clearly identify safety issues. Right then, right now, there’s a sense of urgency in that and understanding of what they needed for the support of their work."
Cooper explained that tier two is the management of the tier one staff, and that tier three is the senior leadership team. “We meet daily with an eye toward escalating issues. And there’s a spirit of urgency in getting this done. One of the things we also include... is a focus on catching people in moments of excellence, what we call ‘caught being awesome.’”
The time needed to participate in huddles and resolve issues raised in huddles was an obvious concern. To ensure that that this is value-added time, “Let’s have a conversation about restructuring and repackaging that time in a way that is more focused and more rapidly responsive. And that’s what the tiered structure gave us, a mechanism to put that in place.”
Below is an illustration from a slide that Cooper used, showing a board. The text is not easy to read, but it starts with "Commit to Zero" and "Outcome and Process Measures" on top.
Those measures categories are:
- Patient Harm
- Employee Harm
- Visitor Harm
- Admit > 24 hrs
- Staffing
- Patient Risk
- Employee Risk
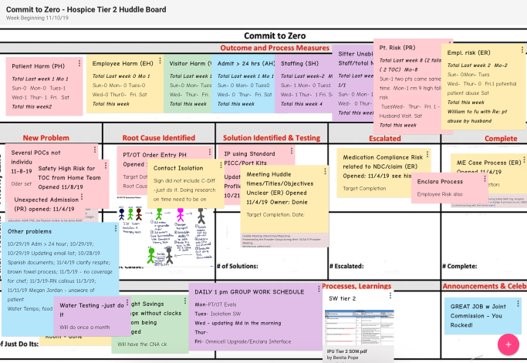
The board then includes spaces for the flow of ideas from:
- New Problem
- Root Cause Identified
- Solution Identified and Testing
- Escalated
- Complete
“And it does mean that we’re going to clear our calendars at times because there is an escalated issue that trumps whatever we thought we had on our calendar. After that, it’s a change, not only the way we deliver information, but the cadence of our work. And it gets very focused on doing things right now. Information is highly perishable.”
“Quit Doing That” - How DHCH Cut Executive Meeting Time by 65%
The tiered huddle structure yielded great benefits, as well as challenges. That is because staff realized that the huddles provide “'a mechanism to express my concern to escalate an issue for help.' This reveals more problems than you ever thought you had,” Cooper said, which led to a thorough review of the many standing meetings managers and leaders had.
“Every member of our team felt overwhelmed by the time expectations when we started this... We found there were many non-valuable things we met around, and we did something known as ‘quit doing that.’ The fact is we’ve cut our executive meeting time, I said [in the slide] by 50-plus %, but the truth is, it’s closer to 65%.”
The Risks of Over-Estimation and Under-Estimation
One of Cooper’s slides contained a quote from Moliere - “It is not only for what we do that we are held responsible, but also for what we do not do.” Cooper said that this quote is at the top of every leadership agenda. “It’s really about recognizing what we’ve left undone. And I would ask that, do we really under-estimate the risk of the status quo, and over-estimate the risk of taking action? It actually hinders us when we get caught in this process of trying to make it perfect before we implement it, as opposed to recognizing that it is going to be perpetually iterative, and liberate ourselves from trying to define the perfect prior to implementation.”
"I would ask that, do we really under-estimate the risk of the status quo, and over-estimate the risk of taking action? It actually hinders us when we get caught in this process of trying to make it perfect before we implement it, as opposed to recognizing that it is going to be perpetually iterative."
Broken Processes Break Staff Engagement and Endanger the Commitment to Zero Harm
With input from the safety huddles, DHCH leaders began to better understand “what our staff needs were and trusting the intentions of the people involved. We quit blaming who was causing the problem and unpacked the broken processes that were causing everyone to struggle, and to be dissatisfied.”
“We reduced our nursing turnover by 50%. 50%, by hearing our frontline staff say, ‘this is burdensome. I hate this.’ It’s authentic feedback, and we needed to hear it. And we improve the way we deliver care. Our staff is expressing far greater satisfaction... They understand the process they’re going through because they helped design the changes. They know they were part of the solution. That in itself leads to cultural change. Our frontline staff is engaged. There is a baked-in mechanism for engaging them every day.”
The Fundamental Shifts that Develop from Respect
“We needed to improve the speed of our decision-making and our responsiveness to the needs of our frontline staff, not only through the escalation process, but through solving things to root. So issues don't emerge and re-emerge and re-emerge, until slowly we grind people down.”
“This is a fundamental shift in the way we begin to think, solve problems, turn our staff into problem-solvers and cease being the problem-solvers ourselves. It’s a fundamental shift in the way we begin to think, lead and engage. If you’re going to do this, you have to be fully committed, you can’t go part of the way.”
“The biggest barrier for me was not solving things or trying to solve them the way I have before. I’ve always thought of myself, my value was what I knew. 'I’m going to be an accumulator of knowledge, and that’s the value that I bring.' This has really begun to shift my self-view as a leader, to think of myself as a perpetual learner and then a perpetual adapter. And that my role is to coach and shift my knowledge base to others.”
"This has really begun to shift my self-view as a leader, to think of myself as a perpetual learner and then a perpetual adapter. And that my role is to coach and shift my knowledge base to others.”
“You really need to fully commit and get to the other side of changing the way we think, what you thought you knew probably doesn’t matter. You may want to check that at the door. If you tend to be encumbered by a pretty large ego, I would encourage you to check that at the door as well, because there’s some pretty humbling experiences that go on through this. As you make yourself a member of the team and a coach and pull yourself out of a hierarchical leadership role that we’ve often been baked into for years.”
“Get ready for a mess, it’s coming, but our staff are already dealing with messes and they want our help. If we can get in there with them, it turns out they can actually help us solve them, and solve them quickly.”
Questions and Answers
Below are just a few of the questions submitted during the webinar, and Cooper's responses.
QUESTION: When you talk about encouraging people to speak up, to point out risks, or near misses or worst case, harm, what are some things that you and other leaders do to make it safe for people to speak up about that?
COOPER: I think you can tell people all sorts of stuff, 'Hey, we're not, you know, we want to hear your voice.' That's important. The words should match it. But ultimately it's our behaviors as leaders that are going to define a culture of whether people feel safe. Part of it is going out and seeing what happens. Too often, I think we get relegated to our offices, to our Zooms, to meetings with a group of us that are always meeting together. As some subset of your leadership team is always together. And to set that down and make part of our daily job to go be with our frontline staff. And that presence, that familiarity begins to break down some of the barriers that our organizational charts unfortunately create.
"Ultimately it's our behaviors as leaders that are going to define a culture of whether people feel safe."
If I show up on a tier one huddle, no one's surprised anymore because that's what I do. 'Well, Cooper, do you have anything to say? No, I came to listen.' I tell everybody good morning, but I really came here to hear what's going on at frontline. And if it's a direct care setting, you're there. And so you start having this engagement and soon people quit paying attention to whose job title it is, who from what level in the organization is on this tier, walking this floor and showing up in this meeting. And it really becomes, we all go to each other's work and we all learn from each other. And suddenly it's a subconscious change in culture. It's subtle, but it's powerful. And then people start telling you stuff.
QUESTION: One of the things that struck me about you, Benita [Benita Pope, Director of Hospice Services] and your team, how you've built and use the system of continuous improvement, is how it's allowed you to get people away from trade-off thinking. In other words, if we pursue one goal, that's good. We have to set aside another goal or there's trade-offs, and instead realizing that making processes great allows good things, all of these good things to happen at the same time. What are your thoughts about that observation?
COOPER: Well, I think sometimes we forget we're making trade-offs by our inaction, and that was really what I meant earlier, by do we overestimate the risk of change and underestimate the risk of the status quo. We're making trade-offs that are not intentional, but they come through just accepting them. The static inertia has a trade-off and often it's terrible. If we look at the impact on our staff and our patients, we also look at the impact on our organization's bottom line.
"I think sometimes we forget we're making trade-offs by our inaction, and that was really what I meant earlier, by do we overestimate the risk of change and underestimate the risk of the status quo. We're making trade-offs that are not intentional, but they come through just accepting them. The static inertia has a trade-off and often it's terrible."
So when we think about that, these trade-offs, realize there aren't as many trade-offs, we're often falsely creating that. And if we can embrace change that's fed by scientific thinking and from frontline experience, we will accomplish many positive results at the same time. There is still a need to prioritize. When we started being overwhelmed with all these ideas coming forward, we knew we couldn't do them all at once. As a leadership team, we created a series of four priorities that we actually keep at the top of the agenda from every leadership team, that and the quote from Moliere, that we use to make decisions.
Because we're going to have to make some tough decisions and we need to come to agreement on what those priorities are as a team. Not whimsically, what's, not what's, today's motivation, not what was on my mind when I woke up this morning. Or the last email I got from the large health system. What are our priorities as an organization that we can agree on and use those to help us figure out where we're going to place our resources next.
QUESTION: Back to the beginning of this journey with the organization, did you provide training to all levels on Lean and other concepts to start?
COOPER: Yes, we did provide training. One of the things that we did, and I think this was actually through the coaching of your team, Mark, of your folks at Value Capture, was our leadership team went through training at multiple levels of the [Duke University Health] System, but also here locally. The hard part then became that we had to become our staff's trainers. You think you know something until you have to teach them, and then you truly begin to learn it. I think most of us have experienced that.
So by putting ourselves in the uncomfortable role of trying to learn and then become the teachers and coaches for our staff, it did two things. It one, made us learn it better. The other, it created immediate buy-in. Someone else isn't coming to our program and telling us what to do. We are doing this ourselves.
QUESTION: You see in a lot of places where someone's maybe brought in from the outside to train
the frontline staff, and then at some point, hoping to influence leaders. And I would share, you know, the observation of the hypothesis that plays out, that it's more effective to have something be leader-led, coached through that, right? Can you share a little more?
COOPER: It has to be an internal locus of control. You can't have somebody come in and do this for you. The difference again between the consultant and the coach. The coach helps you do it. The consultant does it. This had to be ours, because at some point your coach or consultant, your outside party is going to say, okay guys, there's nothing we can do, we're going home. Now we have to keep that living and alive. We have to figure out how to refine it and make it better next year than it is this year. That's ours. There has to be absolute ownership in this and that ownership turns into engagement. And also we always talk, how do we get staff buy-in? If the staff are doing it, you don't have to ask how to get staff buy-in. The staff's bought in, they're the ones doing it. You don't have to get them to like your idea. It's their idea.
QUESTION: How did you know your organization was ready for this work? How much of that was the thought process? Are you ever ready? Or at some point you just have to go?
COOPER: I think we can overanalyze that. I think sometimes trying to get ready as an unintentional way to avoid embracing change. I just need to be ready enough. Well, when are you just, 'it's time to do it,' because you're never going to be ready."Your status quo is not effective. If it's not working well now, you're ready for making it right. What are you waiting on?"
If you'd like to hear more from Cooper Linton in "Applications of Lean Leadership Methods in Home-Based Care," and access the slides and transcript, click the image below. You can also listen to our Habitual Excellence podcast episode with Cooper Linton, Benita Pope, and Value Capture Senior Advisor, Mike Radtke as the host.
Additionally, you can also learn more about the great work at DHCH in our white paper, "Continuous Learning Leads to Continuous Improvement."
If you would like to learn more about Value Capture and our coaching approach to support leaders in their performance transformation, please complete our Contact Form.

Written by Melissa Moore
Ms. Moore’s responsibilities center on marketing and communications. Prior to joining Value Capture, she served as a Marketing Manager at Reed Smith, a global law firm. Other career steps include: co-founding and operating a trend-setting coffeehouse; securities lawyer; and, service and equipment sales.




Submit a comment