A warning for health care leaders comes from two sources, one familiar, one less so.
The first is the representative front-line RN who wrote an op-ed recently in a national newspaper noting that “she thought more would have changed by now” in her health system as a result of the learnings of the pandemic.
The less familiar source comes via historians who have noted, with surprise, the extremely small amount of reflection and writing about the devasting 1917 pandemic that exists in the historical record.
Why is there so little written about this individual and collective trauma a century ago?
The leading hypothesis is that everyone wanted to forget what they had been through – too disturbing, too difficult – and get on with their lives and work.
We can sympathize, but what lessons were lost, what lessons are forgotten?
Today, as we enter the COVID-cliff period of the pandemic, American health care leaders face a choice -- to forget and do damage, or to heed and to change things powerfully for the better.
Of concern, amid the latest huge challenges, including fiscal crises driven by staffing crises -- many are reacting with some of the “same old” leadership behaviors, including across-the-board staffing and service cuts.
Trying to cut our way to health was a big mistake in the early phase of the pandemic.
A Reversion to Pattern?
Before the pandemic, periodic layoffs were the kind of leadership behavior that traumatized organizations and left huge cultural gaps between leaders and the front line – the gaps that have led to the fiscal spirals, leading to RN and other front-line dissatisfaction.
Instead of more change for the better, it’s a reversion to pattern for our front-line teams, no matter how much we hold them up in our rhetoric, or how many “staffing” initiatives we launch.
Happily, other leaders with more of a systems-building approach to organizational leadership, are deploying powerful approaches to solve the ACTUAL problem in a deep way that builds culture and capabilities instead of destroying them.
A Positive Example
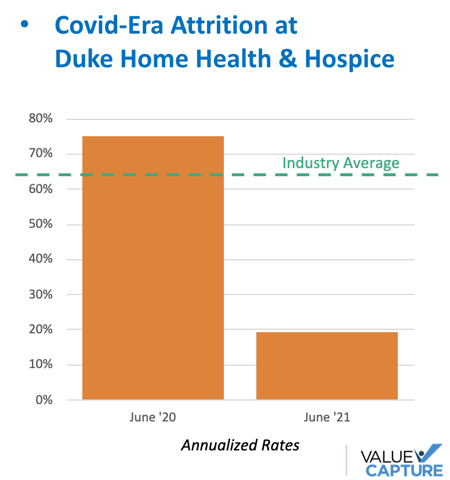
Just one great example is the team at Duke HomeHealth and Hospice, which turned a 75% RN turnover rate (in the teeth of the crisis) to a 19% rate that continues to improve.
From 75% to 19%.
How did they do this?
By digging in and realizing the key tools and systems that the RNs had to use in their daily work were broken. These broken tools and systems were a source of continual frustration and inefficiency.
The organization did the work required to make them better.
They also realized the teams needed their leaders to be much closer to the work and to them, every day. This proximity enables them to help solve problems quickly and spread lessons learned. They built a better management system that did just that.
The RNs feel supported, the problem has dramatically eased, and they are claiming a potential $20 million revenue expansion opportunity in this small division as a result.
Solve the actual problem.
The actual problem was not "staff are leaving." The actual problem was much deeper than that, closer to a root cause that stated that a lack of support (management, improvement, tools, and systems) was causing frustration that drove people to leave.
Do you want to bring your leaders into closer, active support, every day? Learn more about the Duke team’s recent presentations about their accomplishments.
And they'll be sharing more with us (and with you) in a new webinar presentation that we'll be hosting in December. Subscribe to our newsletter to make sure you get notified about how to register:
The Right Approaches That Work
If health care leaders are willing to fight amnesia, they can find great promise in the fact that they have done a lot of the “right thing” in the very recent past. During the teeth of the most harrowing, exhausting waves of COVID, a large percentage of health systems succeeded in important ways because they were FORCED to deploy some of these approaches:
- Leaders rapidly reorienting the organization to what front line staff were facing
- Leaders directly connected to the work
- Rapid experiments to improve via
- Leadership huddles multiple times a day
- Aligning quickly around urgent goals such as standing up telehealth
They were succeeding with blinding speed because of the quick resolution of problems. They quickly provisioned support and they spread news about what was helping.
From Amnesia to a Wake Up Call
One C-suite exec at one of our nation’s most prominent systems shared something profound that struck her during a recent listening session with front-line teams.
Like a good leader, she wanted to get “under the hood” of the challenges she was hearing — of “burnout” and the buzzwords about needing “resilience” from her directors. She needed to investigate since she knew people were back to working regular hours and their staffing had been relatively stable compared to others.
Going straight to the teams and asking them to reflect, she was struck that all of the positive emotions and recommendations stemmed from what they had done together when the crisis was hardest, and the desire to keep it going now. The most negative emotions were associated with the reversion to “pre-covid” behaviors, including returning to having a much greater distance between leaders and front-line teams.
Back then, they said, we were pulling together and working on our actual problems — quickly and together. We were supported.
Are we willing to let that go now just because our lives and our patients' lives are in slightly less peril? Are we willing to fade back from our teams, and through our fiscal decisions, have them believe they have become numbers on a balance sheet to leaders again?
It’s a wake-up call this senior exec is waving and acting on in her c-suite.
We all just proved we can do big things together, fast, to solve our biggest problems, including fiscal problems, by solving the right problems in the right way.
Focus on the actual work (the work system), speed up the pace of problem-solving (the improvement system), and bring leaders closer to enable it all (the leadership system).
Do this for our patients, for the financial health of the organization, and for ourselves.
Now we just have to be willing to remember that we did it and act again on the lessons.




Submit a comment